Flea-borne Typhus
Flea-borne Typhus ICD-9 081; ICD-10 A75 (Murine Typhus, Endemic Typhus)
Flea-borne Typhus, (Murine Typhus, Endemic Typhus)
Flea-borne (also known as “murine” or “endemic”) typhus is a rickettsial disease caused by Rickettsia typhi. Infected fleas carried by rats, opossums, cats, dogs, and other small mammals can spread these bacteria. The disease is like louse-borne typhus (R. prowazekii) but is generally milder. Disease onset is often sudden, and symptoms may include fever, headache, chills, weakness, nausea/vomiting, body aches, and rash. Flea-borne typhus can be a serious disease and can result in hospitalization. This is more likely with delayed diagnosis and treatment.
General Information and Resources
Rats and their fleas are the natural reservoirs (animals that both maintain and transmit the disease organism) for flea-borne typhus. Other animals, such as opossums and domestic cats, may also transmit of flea-borne typhus. Fleas, such as the rat flea, Xenopsylla cheopis, and the cat flea, Ctenocephalides felis, are the most common vectors (animals that transfer the disease from one host to another) of flea-borne typhus.
People get flea-borne typhus from an infected flea. Most fleas defecate while biting. The feces of infected fleas contain the rickettsial organism. The rickettsiae enter the body through the bite wound or from a person scratching the bite area. It is possible to get flea-borne typhus by inhaling contaminated, dried flea feces. However, this method of transmission is not as common as transmission from a biting flea.
The incubation period for flea-borne typhus is 6-14 days. Symptoms of the disease include headache, fever, nausea, and body aches. Five or six days after symptoms begin you may get a rash that starts on the trunk of your body and spreads to your arms and legs. If left untreated, the disease may last for several months. A doctor can conduct tests to tell you if you have flea-borne typhus.
The best way to protect yourself and your family from flea-borne typhus is to:
- Clean your yard so that rodents, opossums, and stray cats cannot live there.
- Remove any brush or trash, keep the grass mowed, and keep firewood off the ground.
- Do not leave pet food out at night as this attracts other animals.
- Prevent rodents from living in your house.
- Treat for fleas before you begin rodent control in your house or yard. Otherwise, when the rodents die, the fleas will search for new hosts, possibly you and your family. There are several commercial flea control products on the market. Pick one and follow the label instructions.
- If you own pets, control the fleas on them regularly. If they come in contact with infected fleas, they could bring them home to you. Ask a veterinarian about flea control products that are safe to use on your pets.
If you suspect that you have flea-borne typhus, see a doctor as soon as possible. If you wait too long to see a doctor, you may have to be hospitalized. Flea-borne typhus is easily treated with certain antibiotics. Once you recover, you will not get it again.
If you have more questions about flea-borne typhus or flea control, consult with a physician or a veterinarian. Questions can also be answered by your local health department or the Texas Department of State Health Services, Zoonosis Control Branch.
Healthcare Providers
Report Typhus within one week » Form
There are several laws in Texas (Tex. Health & Safety Code, Chapters 81, 84, and 87) that require healthcare providers, hospitals, schools, and labs to inform the Texas Department of State Health Services (DSHS) if they think someone has a notifiable condition (25 Tex. Admin. Code §97.2).
In the United States, Texas reports the highest number of flea-borne typhus cases annually. Most of the murine typhus cases in Texas occur in South Texas from Nueces County southward to the Rio Grande Valley. In the past 15 years, case counts have drastically increased and new areas of endemicity have emerged in the Dallas-Fort Worth metroplex, Greater Houston area, Bexar, Travis, and other Texas counties.
Over 5,800 cases of flea-borne typhus were reported between 2008 and 2022 [max = 738 cases/year (2018); min = 135 cases/year (2010)] (PDF). Approximately 70% of the cases were hospitalized and 13 cases were fatal.
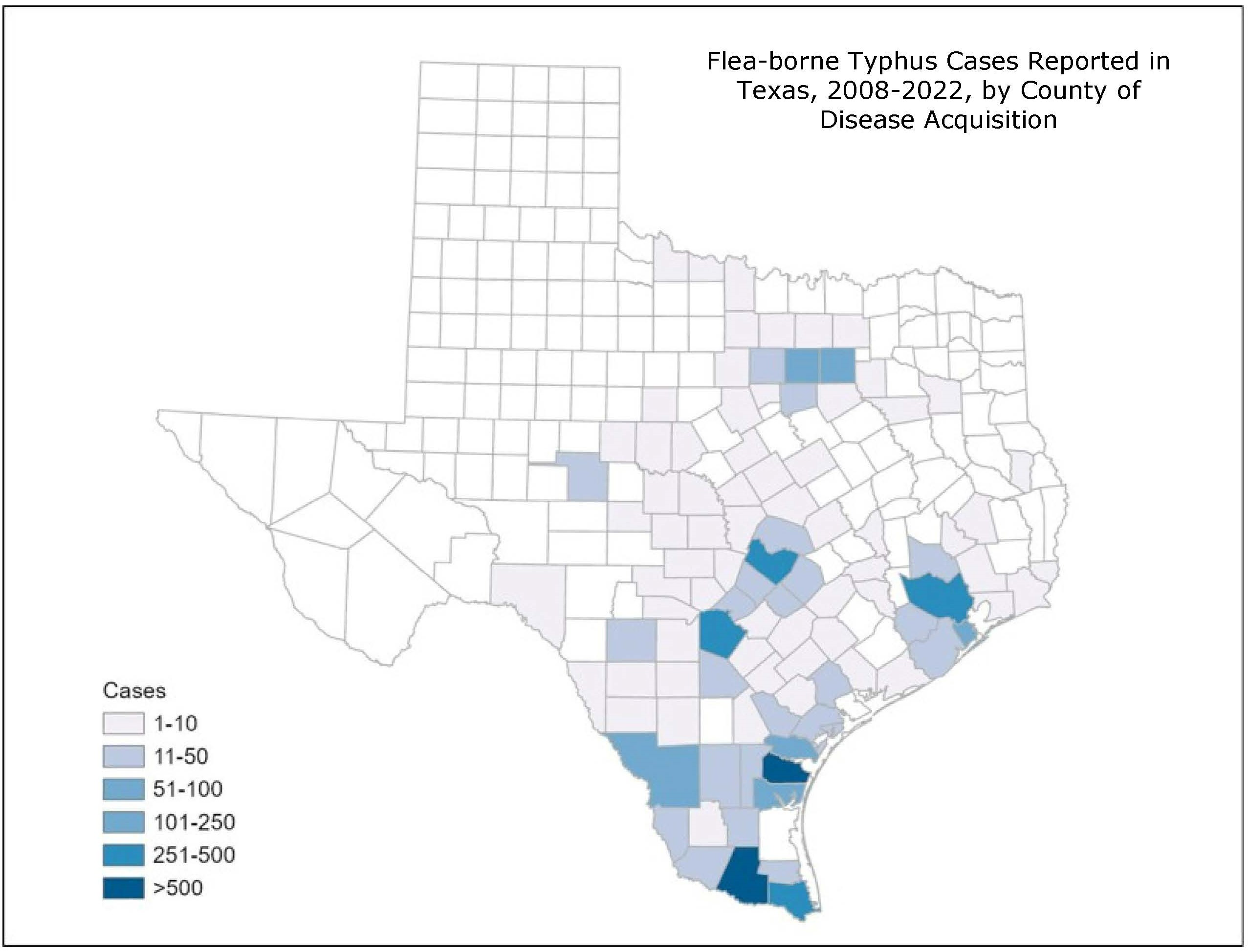
Flea-borne Typhus Cases Reported in Texas, 2008-2022, by County of Disease Acquisition. Cases where area of acquisition is unknown are excluded from map (n=4430).
People with typhus report non-specific symptoms including fever, headache, chills, malaise, anorexia, myalgia, rash, nausea, and vomiting. Laboratory findings may include thrombocytopenia, hyponatremia, elevated hepatic transaminases, and CSF abnormalities consistent with aseptic meningitis. Although flea-borne typhus is often a relatively mild, self-limited illness, more than 60% of reported cases are hospitalized. When left untreated, severe illness can cause damage to one or more organs, including the liver, kidneys, heart, lungs, and brain. As with other rickettsial infections, prompt antibiotic treatment is recommended; treatment should not be delayed pending diagnostic tests.
Laboratory testing is required to confirm a diagnosis of flea-borne typhus. The most efficient and readily available diagnostic method to confirm infection with R. typhi is the detection of IgG antibodies to R. typhi using an indirect fluorescent antibody (IFA) test in acute and convalescent serum specimens collected at least 3 weeks apart However, because antibodies for rickettsial diseases can be cross-reactive, specimens should be tested against a panel of Rickettsia antigens, including, at a minimum, R. rickettsii and R. typhi, to differentiate between the spotted fever group and non-spotted fever group Rickettsia spp. Many commercial laboratories offer rickettsial serology testing, but it should be noted that ELISA or EIA tests are not reliable for rickettsial disease diagnosis. Also, antibodies are typically not detectable until about 7 days after illness onset, so a negative test result on a sample taken prior to a week after illness onset does not rule out rickettsial infection (repeat testing after this time is critical to confirm or rule out infection). Molecular testing is a more definitive testing option for acute infection. Whole blood collected within a few days of illness onset may be tested by PCR in an attempt to detect Rickettsia spp. Samples may be routed through DSHS to CDC for Rickettsia Molecular Detection.
- Typhus Fevers Centers for Disease Control and Prevention
- Rickettsial Diseases Centers for Disease Control and Prevention, Yellow Book 2024
- History, Rats, Fleas, and Opossums: The Ascendency of Flea-Borne Typhus in the United States, 1910–1944
- Fatal Flea-Borne Typhus in Texas: A Retrospective Case Series, 1985–2015
- Typhus Group Rickettsiosis, Texas, USA, 2003–2013
Links to external sites are intended to be informational and do not have the endorsement of the Texas Department of State Health Services. These sites may also not be accessible to persons with disabilities.
Mailing Address
Department of State Health Services
Zoonosis Control Branch
PO BOX 149347 - Mail Code: 1956
Austin, TX 78714-9347
United States
Physical Address
Department of State Health Services
Zoonosis Control Branch
1100 W. 49th Street, Suite T-502
Austin, TX 78756-3199
United States